Polycystic ovarian syndrome affects 1 in 5 women making it one of the most common hormonal conditions experienced by females (1). Its consequences can appear alarming and many women may feel quite hopeless as far as managing the condition is concerned. However, its highly responsive to nutritional intervention and here’s why:
First, a brief look at PCOS. For a diagnosis to be made, 2 of the 3 criteria (2) must be satisfied:
-absence of a regular period
-evidence of hyperandrogenism (that’s high testosterone)
-the detection of cysts on the ovaries when viewed on ultrasound
Other consequences are metabolic, cardiovascular and hormonal in nature and generally include the following:
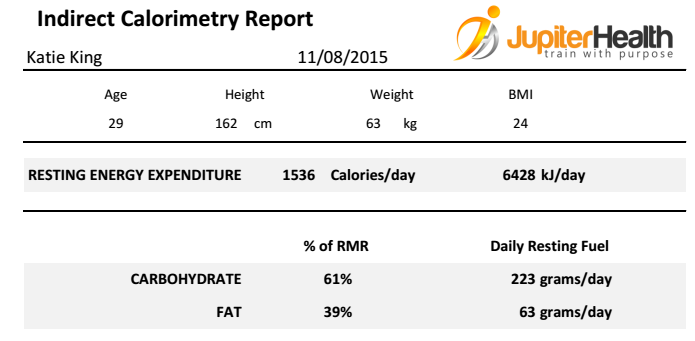
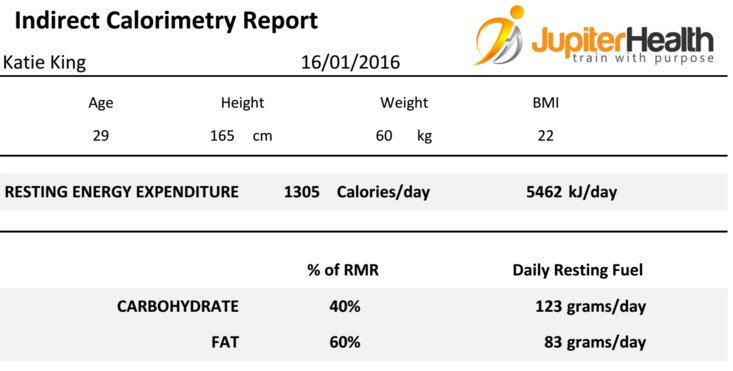
-reduced insulin sensitivity: women with PCOS seem to have up to 40% reduced insulin uptake when compared with non-PCOS women. I.e. the ability to handle simple carbohydrates is significantly reduced, much like type 2 diabetes.
-increased circulating insulin can drive up central adiposity; i.e. fat around the waist. In general, weight management is usually more difficult for women with PCOS.
-higher cardiovascular risk factors; cholesterol, blood pressure and homocysteine to name a few, are more likely to be sub optimal. This is a cumulative effect of higher blood sugars, unbalanced hormones and increased central fat: all drive up systemic inflammation.
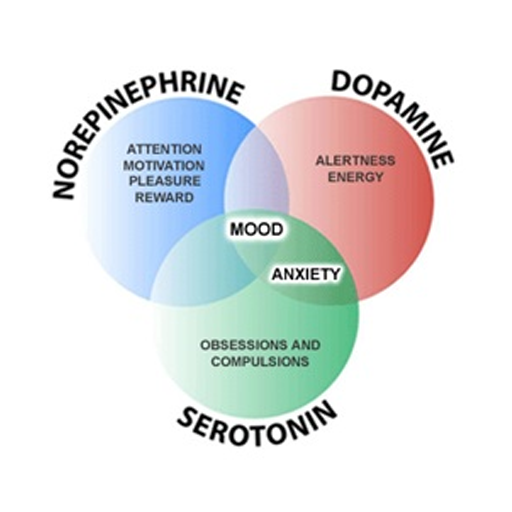
-Compromised mental health including higher incidences of depression and anxiety. Likely a cumulative effect of higher systemic inflammation and out of whack hormones.
What does PCOS have to do with Nutrition?
A lot actually. PCOS is sometimes referred to as ‘diabetes of the ovaries’ so considering the diet will go a long way in managing the condition. We can reduce insulin resistance by including adequate protein and healthy fats alongside fibre rich, unrefined carbohydrates with each meal. A women with PCOS is NOT going to thrive on a low fat diet.
Improving blood sugar and insulin sensitivity may assist with weight management. This may in turn have a positive effect on lowering inflammation which will improve cardiovascular risk factors and support healthy mental health.
Plus, there’s loads of research as far as specific nutrients and nutritional medicine* is concerned. Here are some of the tools we have in our belts:
-N acetylcysteine a naturally occurring amino acid taken at certain dosages assists with ovulation and fertility in women with PCOS. View the full meta-analysis here.
-Inositol, (an often forgotten B vitamin) currently one of my favourite supplements in clinic can reduce elevated testosterone levels and improve insulin levels as shown in many papers including this one here.
-Neurotransmitter support such as natural GABA, 5 hydroxy-tryptophan (precursor for serotonin) and SAMe are viable and important options for PCOS sufferers seeking mental health support without side effects.
This represents the tip of the iceberg and takes a birds eye view on a condition that may vary from person to person. The drivers are more complicated than this article allows, but the take home point is: PCOS is not a ticket to infertility. There is hope outside of the contraceptive pill, IVF and diet shakes which may work for some women, but result in suffering and side effects for others. You deserve to know your body, understand your condition and know your options.
*Don’t take herbs or supplements without consultation with a practitioner. They can interact with medications so should be used with caution and prescribed by a professional. Don’t purchase herbs and supplements over the internet as they may not be regulated by the TGA (Australia’s supplement ‘watchdog’) and they may not be formulated to therapeutic strengths or formulas.
REFERENCES
- Statistics from Royal Australian College of General Practitioners, webpage available here.
- The Diagnosis of Polycystic Ovarian Syndrome in Adolescents, available here.
- N-acetyl Cysteine for Polycystic Ovarian Syndrome : A systematic Review and meta-analysis of Randomised Controlled Clinical Trials. Available here.
- Metabolic and Hormonal Effects of myo-inositol in women with polycystic ovaries, available here.